Effects of High Blood Pressure
Effects of High Blood Pressure

Introduction
High blood pressure, medically termed hypertension, is a chronic condition characterized by persistently elevated blood pressure levels in the arteries. It is often referred to as the "silent killer" due to its typically asymptomatic nature in the early stages, allowing it to gradually damage vital organs over time. According to the World Health Organization (WHO), hypertension affects over 1.28 billion adults worldwide, with the majority living in low- and middle-income countries. A blood pressure reading of 130/80 mmHg or higher is now classified as hypertension, reflecting the updated guidelines that emphasize earlier intervention. This article explores the multifaceted effects of high blood pressure on various organ systems, quality of life, and societal health, highlighting its role as a major global health burden.
Table of Contents:
1.Effects on the Cardiovascular System
2.Effects on the Renal System
3.Effects on the Central Nervous System
4.Effects on the Ophthalmic System
5.Effects on Quality of Life and Mental Health
6.Economic and Societal Impact
7.Conclusion
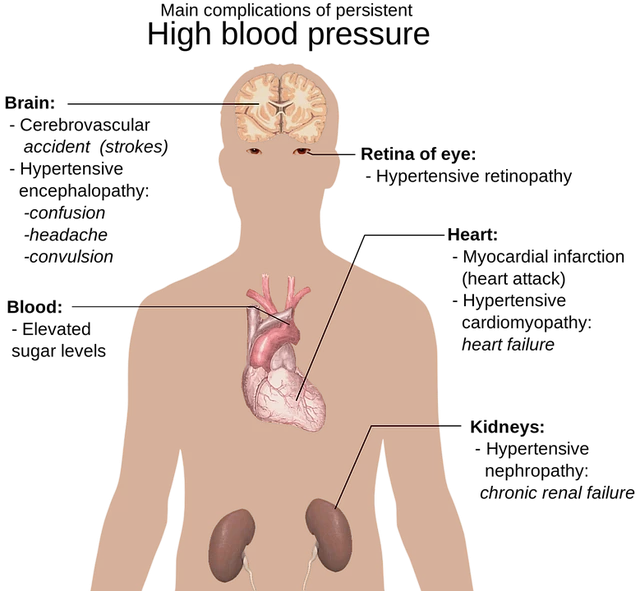
1.Effects on the Cardiovascular System
1.1. Impact on the Heart
The heart is one of the primary organs affected by hypertension. When blood pressure is consistently high, the heart, particularly the left ventricle, must work harder to pump blood against the increased resistance in the arteries. This prolonged overexertion leads to left ventricular hypertrophy (LVH), a condition where the heart muscle thickens. While the heart initially compensates by strengthening, LVH weakens its long-term efficiency, reducing the ventricle's ability to fill with blood and pump it effectively. Over time, this can progress to heart failure, a life-threatening condition where the heart cannot meet the body's oxygen and nutrient demands.
Hypertension also significantly increases the risk of coronary artery disease (CAD). The high-pressure blood flow damages the inner lining of coronary arteries, promoting the accumulation of fatty deposits (atherosclerosis). These plaques narrow the arteries, reducing blood flow to the heart muscle and causing chest pain (angina). If a plaque ruptures, it can form a blood clot, leading to a myocardial infarction (heart attack). Studies have shown that individuals with hypertension have a two- to threefold higher risk of developing CAD compared to those with normal blood pressure.
Additionally, hypertension is a major contributor to arrhythmias, particularly atrial fibrillation (AFib). The structural changes in the heart due to LVH and the electrical disturbances caused by chronic stress on cardiac tissue increase the likelihood of irregular heartbeats. AFib not only impairs heart function but also raises the risk of stroke by fivefold due to blood clot formation in the heart.
1.2. Impact on Blood Vessels
High blood pressure damages the endothelial cells that line blood vessels, triggering a cascade of pathological changes. The primary vascular effect is arteriosclerosis, the thickening and stiffening of arterial walls. As arteries lose their elasticity, they are less able to expand and contract with each heartbeat, further elevating blood pressure in a dangerous feedback loop.
In the aorta, the body's largest artery, chronic hypertension can lead to the formation of aneurysms, weakened bulges in the vessel wall that may rupture, causing life-threatening internal bleeding. Aortic aneurysms are particularly lethal, with a mortality rate exceeding 80% if they rupture.
Peripheral arteries, such as those in the legs and arms, are also affected. Peripheral artery disease (PAD) occurs when atherosclerosis narrows these arteries, reducing blood flow to the extremities. Symptoms include pain during walking (claudication), numbness, and in severe cases, tissue death (gangrene) that may require amputation. PAD is strongly associated with hypertension, increasing the risk of cardiovascular events like heart attack and stroke by two to three times.
2.Effects on the Renal System
The kidneys play a crucial role in regulating blood pressure by filtering waste and excess fluid from the blood. Conversely, hypertension causes significant damage to the renal system, creating a vicious cycle where kidney dysfunction worsens blood pressure control.
2.1. Renal Artery Damage
High blood pressure affects the small arteries within the kidneys, leading to hyaline arteriolosclerosis, a condition where the walls of the arterioles thicken and harden due to protein deposition. This reduces blood flow to the nephrons, the functional units of the kidney, impairing their ability to filter blood effectively. As nephrons are progressively destroyed, the kidneys lose their regulatory capacity, leading to fluid retention that further elevates blood pressure.
2.2. Proteinuria and Kidney Failure
Damage to the glomeruli, the tiny filters in the nephrons, causes proteinuria (excess protein in urine), an early sign of kidney dysfunction. Persistent proteinuria indicates that the glomeruli are no longer able to retain proteins, which can lead to swelling (edema) and further kidney damage. Over time, untreated hypertension progresses to chronic kidney disease (CKD), with up to 25% of end-stage renal disease cases linked to hypertension. CKD patients often require dialysis or a kidney transplant, with hypertension significantly reducing their survival prognosis.
3.Effects on the Central Nervous System
3.1. Stroke Risk
Hypertension is the single most important modifiable risk factor for stroke, accounting for nearly 50% of all stroke cases. It damages the blood vessels in the brain in two primary ways:
- Ischemic Stroke: Atherosclerosis in cerebral arteries, combined with high pressure, can lead to clot formation or blockage, depriving brain tissue of oxygen.
- Hemorrhagic Stroke: Weakened cerebral arteries, such as those affected by microaneurysms, may rupture due to the force of high blood pressure, causing internal bleeding in the brain.
Both types of stroke can result in permanent disability, including paralysis, speech impairment, and cognitive deficits, or even death. Even mild hypertension doubles the risk of ischemic stroke, while severe hypertension increases the risk by up to seven times.
3.2. Cognitive Impairment and Dementia
Chronic hypertension also affects brain health by reducing blood flow and causing small-vessel damage. This leads to vascular cognitive impairment, characterized by memory loss, difficulty concentrating, and slower thinking. Over time, these changes can progress to vascular dementia, the second most common form of dementia after Alzheimer's disease. Hypertension also exacerbates the risk of Alzheimer's disease by promoting amyloid plaque buildup and neuronal damage, highlighting its role in multiple pathways of brain degeneration.
4.Effects on the Ophthalmic System
The eyes are not immune to the effects of hypertension, as the retinal blood vessels are highly susceptible to pressure-related damage. Hypertensive retinopathy is a common complication, diagnosed through eye exams that reveal changes such as retinal artery narrowing, hemorrhages, exudates (fluid leaks), and swelling of the optic nerve (papilledema). These changes can lead to blurred vision, visual field loss, and in severe cases, blindness.
Diabetic patients with hypertension are at particularly high risk of diabetic retinopathy, with hypertension accelerating the progression of retinal damage caused by diabetes. Even in non-diabetic individuals, long-term hypertension doubles the risk of vision loss, emphasizing the need for regular eye screenings in hypertensive patients.
5.Effects on Quality of Life and Mental Health
5.1. Physical and Emotional Symptoms
While hypertension is often asymptomatic, uncontrolled high blood pressure can cause symptoms like headaches, dizziness, shortness of breath, and fatigue, which impair daily activities. As the disease progresses and complications arise, such as heart failure or stroke, patients may experience mobility limitations, chronic pain, and dependence on others for care, significantly reducing their quality of life.
5.2. Mental Health Implications
Hypertension is closely linked to mental health disorders, particularly anxiety and depression. The chronic nature of the condition, fear of complications, and the burden of managing medications and lifestyle changes contribute to psychological stress. Conversely, mental health issues can exacerbate hypertension through mechanisms like increased sympathetic nervous system activity and poor adherence to treatment, creating a bidirectional relationship.
5.3. Sexual Dysfunction
Both men and women with hypertension may experience sexual dysfunction. In men, hypertension damages the blood vessels in the penis, leading to erectile dysfunction (ED), while in women, it can cause reduced libido and difficulty achieving orgasm. Antihypertensive medications, such as beta-blockers, may also contribute to these issues, highlighting the need for personalized treatment plans that balance efficacy and quality of life.
6.Economic and Societal Impact
6.1. Healthcare Costs
Hypertension imposes a substantial economic burden due to its high prevalence and association with costly complications. Treating heart disease, stroke, kidney failure, and other hypertension-related conditions accounts for a significant portion of healthcare budgets globally. In the United States alone, hypertension-related healthcare costs exceed $130 billion annually, including direct medical expenses and indirect costs from lost productivity.
6.2. Productivity Loss
Workers with hypertension often experience reduced productivity due to illness, disability, or frequent medical appointments. Premature death from hypertension-related causes further deprives societies of their workforce, particularly affecting middle-aged individuals who are in their prime working years. This economic impact is most severe in developing countries, where healthcare resources are limited and preventive measures are often lacking.

7.Conclusion
High blood pressure is a systemic disease with far-reaching consequences that extend beyond the cardiovascular system, impacting the kidneys, brain, eyes, and quality of life. Its insidious nature, combined with its high prevalence, makes it a critical public health priority. The effects of hypertension are largely preventable and manageable through early detection, lifestyle modifications (such as diet, exercise, and stress management), and appropriate medical intervention. Healthcare providers must emphasize regular blood pressure screenings and patient education to address the silent progression of this disease.
On a societal level, policies promoting healthy environments, affordable medications, and access to healthcare are essential in mitigating the global burden of hypertension. By understanding the multifaceted impacts of high blood pressure, individuals and communities can take proactive steps to protect their health and well-being, turning the tide against this silent but deadly adversary.
In an era where non-communicable diseases dominate global health challenges, hypertension stands as a key target for intervention. Its management requires a collaborative effort between healthcare systems, policymakers, and individuals, underscoring the importance of prioritizing cardiovascular health for a healthier, more resilient society.